Company News - 2024-06-01 08:56
Pharmaceutical Warranties:
A Compelling New Use Case for Interoperability
Obstacles to interoperability have been discussed and debated. But maybe there's a problem with the use cases proposed for interoperability, too — are they compelling enough to drive widespread interoperation?
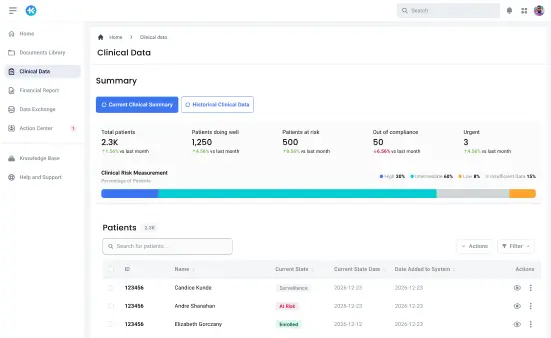
At KlearTrust, we're building tools to support the real-time operation & adjudication of pharmaceutical warranties, which we think represent a powerful and financially sustainable rationale for the exchange of detailed clinical data. We think we can participate in the next wave of interoperability and help drive the industry forward.
Interoperability has been hailed as a significant advancement in healthcare delivery, promising enhancements in patient care along with substantial financial gains. A study conducted in 2014 projected potential annual savings of $78 billion through widespread adoption of data exchange standards. In that same year, the publication of the first version of the Fast Healthcare Interoperability Resources (FHIR) standard provided the industry with a widely accepted framework for data exchange.
However, a decade later, the anticipated benefits of interoperability remain elusive. While the FHIR standard has evolved into a robust framework that has been embraced and mandated by regulators, as well as broadly implemented by provider and payer systems, genuine interoperation — real use of shared patient data for clinical and business purposes — has been limited.
Why has interoperability disappointed?
Healthcare trade journal articles and conference presentations typically cite the same factors as contributors to this shortfall. The self-interest of electronic medical record (EMR) vendors is said to be a key issue, where competitive pressures lead to information blocking practices intended to prevent customers from transitioning to alternative software solutions. Providers are thought to have proprietary interests in patient data as well, particularly within consolidated delivery systems which prioritize control of all steps of the patient journey. Regulators are criticized for not sufficiently mandating or incentivizing compliance with industry standards.
Although these factors are significant, historical evidence suggests that true interoperation develops organically when driven by compelling use cases. For instance, before the establishment of standards for the submission of medical and pharmacy claims, a great deal of claims data was exchanged using a variety of formats and media. Despite the obstacles, clear financial and operational incentives drove the exchange of computable data. This historical context underscores the pivotal role of use cases that cause real interoperation to take hold and grow.
Interestingly, the 2014 study projecting $78 billion in annual benefit described the source of those benefits primarily as “TBD”. It suggested that the elimination of duplicate laboratory tests would be a key contributor to financial benefits. Other sources of benefits are frequently cited in the industry press since then, such as reduced fraud and abuse, or decreased incidence of medical error. It’s not hard, in retrospect, to see the weakness of these use cases and the associated projections — and not surprising that so little interoperation has emerged.
Even before standards were established, providers & payers found ways to exchange medical & pharmacy claims data.
A powerful new use case for interoperability
There is hope, though, that a new class of interoperability-driven applications is emerging that are compelling and valuable enough to instigate meaningful change in the interoperability landscape. A key opportunity is presented by the rapid growth of specialty medications, including cell and gene therapies. Specialty medications now make up more than 50% of total drug spend, and spending continues to increase more than 10% annually.
The rise of specialty medications has ushered in a paradigm shift in the pharmaceutical landscape, presenting unprecedented therapeutic opportunities for patients and providers but formidable business challenges for payers. Specialty medications generally target rare diseases or complex conditions that affect relatively small numbers of patients. While these therapies hold immense promise in improving patient outcomes and quality of life, their astronomical costs and small patient populations pose significant financial burdens for payers. Pricing models associated with specialty medications involve high upfront costs and long-term commitments, requiring payers to grapple with tough decisions regarding coverage criteria, formulary management, and value-based contracting arrangements.
One response to the challenges presented by high-cost specialty medications is the concept of outcomes-based pricing — in effect, pharmaceutical warranties. A pharmaceutical warranty is a value-based agreement that guarantees a specific health outcome for a drug therapy. The manufacturer pays for the warranty. If the drug does not perform according to the agreed-upon metrics, the pharmaceutical manufacturer may offer compensation, refunds, or other financial adjustments. The warranty is designed to share the risk between the pharmaceutical company and the payer, ensuring that the drug delivers the expected clinical benefits and cost-effectiveness.
For payers, outcome-based agreements can mitigate the impact of ineffective treatments and provide a means to manage financial risk while promoting the use of therapies with demonstrated efficacy and value. Manufacturers can use warranties to differentiate their products in the marketplace. By standing behind the performance of their therapies, manufacturers cultivate trust and confidence among healthcare stakeholders. This helps to align incentives with patient outcomes, driving adoption and fostering long-term partnerships. Patients stand to gain from pharmaceutical warranties mainly through improved access to high-value treatments.
The importance of interoperable data
Detailed clinical data, obtained using interoperability tools, plays a pivotal role in assessing patient outcomes and adjudicating claims in outcomes-based arrangements. Unlike traditional reimbursement models, which rely primarily on fee-for-service or volume-based metrics, outcomes-based arrangements prioritize the achievement of specific health outcomes or performance targets. In this context, interoperable clinical data serve as the foundation for evaluating the effectiveness and value of healthcare interventions, providing insights into patient responses, treatment efficacy, and overall care quality.
Interoperable clinical data can also provide a real-time understanding of patient trajectories, from initial diagnosis to treatment outcomes and beyond. Highly granular patient data enables nuanced assessments of individual responses to therapy and empowers stakeholders to track and monitor outcomes over time. It supports informed decision-making regarding treatment adjustments or modifications and allows real-time visibility into financial risk.
The availability of interoperable clinical data is clearly fundamental to the success of any sophisticated pharmaceutical warranty. While early warranty programs were extremely simplistic, often evaluating outcomes in terms of criteria such as discontinuance of therapy, much more sophisticated models are emerging. These will motivate significant advances related to the availability of interoperable data. Practices will have incentives to more thoroughly document observations and therapies, and to improve their use of standard coding. Medical record and claims processing systems will be driven to implement interoperability standards more fully. Solutions will evolve to provide easier connectivity to the variety of medical record systems and to standardize their API's and data.
The future with KlearTrust
At KlearTrust, we’re dedicated to the delivery of sophisticated informatics capabilities and technologies to support the administration of advanced pharmaceutical warranties. We’re confident that the huge (and increasing) share of healthcare spending devoted to high-cost pharmaceuticals and the importance of producing a manageable, sustainable reimbursement model will drive the introduction of ever more-innovative outcomes-based arrangements. These will provide a compelling and valuable use case that will drive interoperability forward.

Ready to Turn Insight Into Impact?
Request a demo today and see how KlearTrust transforms real-world data into real-time results.
Contact us